Published
on
March 16, 2021
| 2,630 views
| 1 follower
members are following updates on this item.
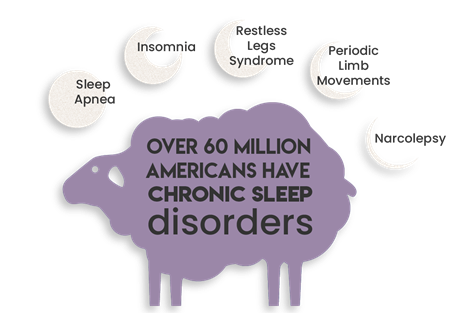
Sleep is vital to your health, safety, and overall well-being. However, disruption of sleep is becoming a prevalent national issue. Over 60 million Americans have chronic sleep disorders, and most adults experience a sleep-related problem, like restless leg syndrome, insomnia, and daytime sleepiness all which have a negative impact on quality of sleep.
 Of those 60 million, 25 million adults suffer from obstructive sleep apnea (OSA), a condition where the upper airway is obstructed during the night. This leads to lower oxygen levels that force the body to have micro-arousals, which are often not perceived by the sufferer but harm the quality of sleep.
Of those 60 million, 25 million adults suffer from obstructive sleep apnea (OSA), a condition where the upper airway is obstructed during the night. This leads to lower oxygen levels that force the body to have micro-arousals, which are often not perceived by the sufferer but harm the quality of sleep.
Untreated OSA contributes to obesity, diabetes, heart issues, and high blood pressure. These conditions are associated with decreased life expectancy. Gastroesophageal reflux disease, or GERD, is more prevalent in suffers of OSA, and can be significantly reduced with treatment of OSA.
Asking your primary care provider (PCP) about sleep issues and having a conversation about your sleep health can start you down a road of treatment that can dramatically improve your quality of sleep, and quality of life.
Here’s what the sleep health journey may look like for you:
 To start your sleep health journey, you may be referred to a sleep specialist for a comprehensive sleep screening, including an in-depth sleep questionnaire and deep dive into your medical history. Your sleep specialist will make sure that you are fully educated on the potential issues or your sleep disorder, and he or she will also ensure that you understand the recommendations in order to pursue diagnosis and treatment.
To start your sleep health journey, you may be referred to a sleep specialist for a comprehensive sleep screening, including an in-depth sleep questionnaire and deep dive into your medical history. Your sleep specialist will make sure that you are fully educated on the potential issues or your sleep disorder, and he or she will also ensure that you understand the recommendations in order to pursue diagnosis and treatment.
 After your comprehensive sleep consultation, a home sleep test or an in-lab test at a sleep disorders center may be ordered. Your PCP may also refer you directly to a sleep lab for the home sleep test or an in-lab test.
After your comprehensive sleep consultation, a home sleep test or an in-lab test at a sleep disorders center may be ordered. Your PCP may also refer you directly to a sleep lab for the home sleep test or an in-lab test.
If you have a home sleep test ordered, typically a registered sleep technologist will instruct you in the use of the device and how to place each element; the single belt that measures breathing effort; the oximeter that measures your oxygen levels; and the nasal cannula that measures your breathing. Just like it sounds, you will take the device home, put it on, go to sleep, then take it off in the morning and return it. The sleep lab will prepare the results for your PCP or sleep specialist.
If you have had an in-lab test ordered, you would schedule a night-time appointment at a sleep lab, which often feature comfortable hotel-styled rooms. The on-site registered sleep technologist will connect several belts to measure breathing effort, several wires to assess brain, muscle, and heart activity, an oximeter and a nasal cannula.
While you snooze, the technologist will be analyzing the quality of your sleep and looking for obstructive sleep apnea and/or other sleep disorders. If obstructive events are observed early enough in the study, the technologist may place you on a positive airway pressure, or PAP, machine during the night. The PAP machine delivers pressurized air through a hose to a mask in order to resolve the obstructive events.
 Depending on the results of your test, whether home or in-lab, your sleep specialist may recommend you return to the sleep lab for a PAP titration test to resolve any observed obstructive events.
Depending on the results of your test, whether home or in-lab, your sleep specialist may recommend you return to the sleep lab for a PAP titration test to resolve any observed obstructive events.
For a PAP Titration, a registered sleep technologist will connect all the monitors as before, plus place you on a positive airway pressure, or PAP, machine. During the night, the technologist will be altering the pressure settings and mode of the PAP unit to custom tailor the best setting that will resolve your obstructive sleep apnea.
 After a successful PAP pressure has been determined, you’ll obtain your PAP device from a home medical equipment company and be instructed on their use. PAP therapy can resolve your obstructive sleep apnea and give you a better night’s sleep. Good sleep health has a ripple effect on overall health, making wearing and using your PAP device imperative.
After a successful PAP pressure has been determined, you’ll obtain your PAP device from a home medical equipment company and be instructed on their use. PAP therapy can resolve your obstructive sleep apnea and give you a better night’s sleep. Good sleep health has a ripple effect on overall health, making wearing and using your PAP device imperative.
However, it is a large adjustment to try to sleep with a mask on your face. Don’t get discouraged if your PAP device isn’t working for you at first - there are dozens of styles for all faces and comforts. Your sleep medicine specialist will work with you and your medical equipment company to help you acclimate to PAP therapy, resolve your sleep apnea, and demonstrate compliance to your insurance company.
As with all things health care, it is always best practice to call your insurance to make sure that all services and devices are covered.
On December 17, 2021, Foundation Health Partners discontinued Sleep Medicine & Sleep Disorders Center services after Dr. Clay Triplehorn's retirement from Tanana Valley Clinic.


Page Options