Published
on
February 24, 2021
| 14,635 views
| 1 follower
members are following updates on this item.

Most often, cold weather injuries affect people who inadequately planned for extreme weather conditions. Cold weather injuries are also caused by ineffective gear, or wearing clothing that are not suitable for the conditions.
Be Prepared
For extended snowmachine or backcountry ski trips, bring back-up layers of gloves, ideally store them in the inner pockets of a jacket so that they stay warm. It is also essential to bring layers of socks, both a thin wicking layer and a wool layer. And of course, appropriate footwear is critical.
It is also a good idea to let friends or family members know your route and expected return date, if taking a prolonged trip outdoors.
If you have a cell phone with you, try to keep it warm and close to the body as possible to keep the battery alive, in case you need it in an emergency. Many backcountry adventurers keep a GPS texting device or satellite phone in an insulated container with activated hand warmers during a trip.
Proper nutrition and hydration are equally imperative. Your body needs adequate nutrition and hydration for blood to flow properly. Local military personnel use an insulating sleeve over a wide mouth 1L water bottle during outdoor training in the extreme cold to maintain hydration and prevent the water from freezing.
Dress for the Conditions
Air trapped between the clothing layers acts as insulation against the cold, so wear several layers of loose, warm clothing. Put on windproof and waterproof outer garments to protect against wind, snow and rain, and be sure to choose undergarments that wick moisture away from your skin, such as polyester, polypropylene, wool, or bamboo materials. Always change out of wet clothing as soon as possible.
Mittens are preferable to gloves, as they provide better protection. Make sure the fit allows space for a thin pain of liner gloves that can offer protection when the outer layer is removed for brief activities that require dexterity in the extreme cold, whether it is pumping gas or attaching your cross country skis.
Trigger finger gloves are a popular compromise between the dexterity of gloves and the warmth of mittens.
Always wear headgear that fully covers your ears. Not only does this protect your vulnerable ears, also reduces the amount of body heat that escapes from your head. Generally a breathable fleece beanie can maintain warmth and keep you dry in low speed/minimal wind activities, whereas a windproof covering is necessary for windy conditions.
Just because you have gear, doesn’t mean you can’t get frostbite. If the conditions are right, frostbite can occur on skin covered by gloves or other clothing. If you feel a body part become cold or numb for more than 15 minutes (usually fingers, toes, ears or nose), stop your activity and warm the body part in an area sheltered from wind.
Signs and Symptoms to Look For
Numbness is the first indication that you need to act and re-warm your extremities. The numbness is a sign that the cold conditions have caused a constriction of the blood vessels and there is no longer adequate blood flow into those extremities.
Fingers, toes, ears, cheeks and even the tip of the nose are frequent areas in the body that lose circulation at a rapid pace, and are typically the areas commonly affected by frostbite.
Stages of Cold Weather Injury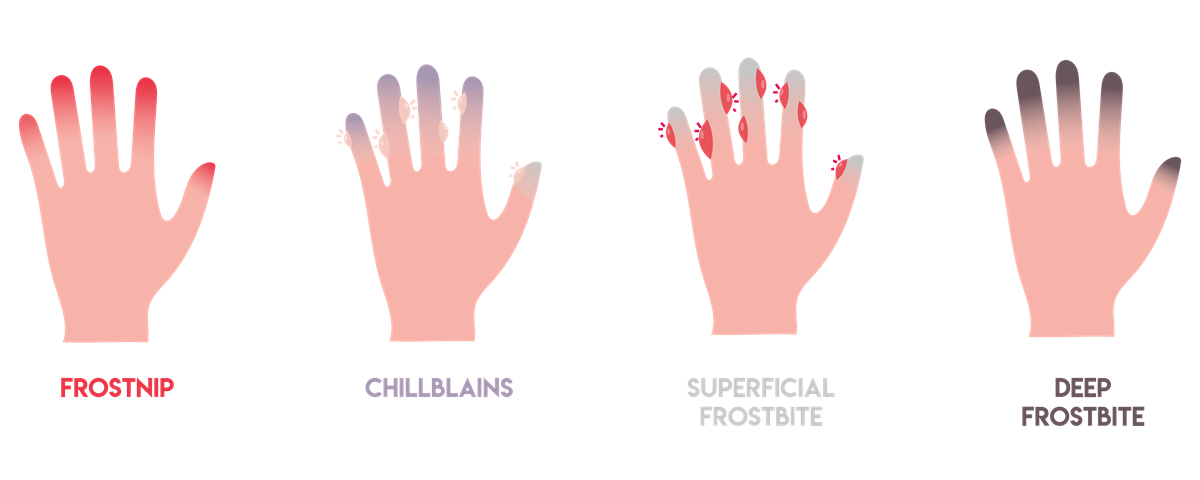
If the numbness lasts too long, which may be different lengths of time for different people, you start having tissue damage. First, your skin becomes very cold and red, then numb, hard and pale.
Frostbite occurs in several stages:
Frostnip. Frostnip, sometimes called cold weather dermatitis, is a mild form of frostbite where freezing of the tissues has not occurred and there is no permanent damage the skin. Continued exposure to cold temperature leads to constriction of blood vessels and thus numbness in the affected area. As your skin warms, you may feel pain and tingling.
Chillblains. Prolonged constriction of blood vessels near the surface of the skin from cold exposure (usually above freezing cold water exposure) can cause damage to the skin, without actual ice crystal formation within the skin. Upon rewarming, redness or blue discoloration of the skin along with a burning or itching sensation and blisters can occur.
Superficial (partial thickness) frostbite. Superficial frostbite appears as reddened skin that becomes white or pale. Ice crystals have formed in the upper layer of the skin. Your skin may begin to feel warm — a sign of serious skin damage. Treatment or rewarming at this stage may cause the surface of your skin to appear mottled and be associated with stinging, burning and swelling. A fluid-filled blister may appear 12 to 36 hours after rewarming the skin.
Deep (full thickness or severe) frostbite. As frostbite and ice crystal formation progresses, it affects all layers of the skin, including the tissues that lie below. You may lose all sensation of cold, pain or discomfort in the affected area, and your skin turns white or bluish gray. Joints or muscles may no longer function. With rewarming, large blisters form 24 to 48 hours after treatment and then the area turns black and hard as the tissue dies.
Risks
Frostbite requires medical attention because it can damage more than just your skin and tissues. Extreme cases can also affect your muscle and bones, and further complications of severe frostbite may include infection and nerve damage, as well.
In the more severe forms, frostbite may require prolonged healing, limiting your ability to participate in outdoor actives for 6 to 12 months. In extreme cases, frostbite can lead to loss of extremities.
What to do
To prevent further injury, warming affected areas will dilate the constricted blood vessels and return blood flow, and thus return oxygen to the tissue. A water bath is often the mode of treatment. If a warm water bath is not accessible, a common solution is to put your hands into the armpits to try to keep them warm.
If possible, try to keep moving. Exercise helps to circulate your blood and keeps your body warm. However, don't do it to the point of exhaustion or if you cannot feel your feet.
To help someone showing signs of hypothermia or frostbite, keep them as warm as possible and call 911. Get emergency medical help if you suspect hypothermia, a condition in which your body loses heat more quickly than it can be produced. A hypothermic individual may be shivering intensely, have loss of coordination, exhibiting drowsiness and experiencing slurred speech.
Seek medical attention if there are signs and symptoms of superficial or deep frostbite, or increased pain, swelling, redness or discharge in the affected area. An over the counter anti-inflammatory medication like ibuprofen or naproxen can reduce pain as well as the severity of tissue damage from a frostbite injury.
What not to do
When numbness occurs and tissue damage is unknown, use caution when warming the affected area with warm water. Approximately 100 degrees is ideal, but realize that higher temp hot of water can cause further damage to the injury. Also avoid warming the area and then exposing it again to the cold. This can cause further injury as well.

Page Options